Every month, VACEP members will share their readings of the latest medical literature. Today, VACEP Board member and University of Virginia Health System emergency physician Joshua Easter, MD, MSc shares data, key points and — where appropriate — his own critique of The Infant Scalp Score: A Validated Tool to Stratify Risk of Traumatic Brain Injury in Infants With Isolated Scalp Hematoma. The study was published in Academic Emergency Medicine on July 16, 2020 by lead author Sara S. Schutzman.
Case: A 6-month-old boy presents to your ED after rolling off the bed onto a hardwood floor two hours ago. He cried immediately after the fall. Since he has consoled and is acting normally to the parents. On physical examination he is alert with no neurologic deficits. He has a 0.5cm hematoma over his occipital region. Do you obtain a brain CT, observe the child in the ED, or discharge him?
Infants with head trauma are difficult to assess in the ED, as they cannot communicate their symptoms. They are at high risk from the radiation associated with CT to identify injuries. Several prediction models assist clinicians with determining the need for CT for these patients. The Pediatric Emergency Care Applied Research Network (PECARN) is the most common model employed in the United States (Kuppermann, Lancet, 2009). Several studies have validated this model’s high diagnostic accuracy for identifying children that harbor very low risk of injury, who can be discharged from the ED. When you apply the PECARN prediction model to the infant in your ED, the patient is classified as moderate risk, and the model recommends observation or CT (Figure 1). This recommendation is less useful than when the model classifies children as low or high risk and provides a definitive recommendation about CT acquisition.
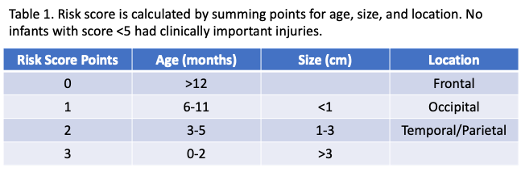
The recent study by Schutzman et al. in Academic Emergency Medicine aimed to provide additional risk stratification for infants falling into this moderate risk category as a result of a scalp hematoma (Schutzman, AEM, 2020). Prior to the publication of the PECARN model, Greenes et al. had derived a risk score for infants with scalp hematomas based on the size and location of the hematoma as well as the infant’s age (Table 1). Younger age, larger hematoma size, and temporal or parietal location harbored higher risk. This derivation study was limited by small sample size.
In the current study, the authors validated the risk score in the 1,289 infants from the PECARN study sample with isolated scalp hematomas and no other concerning signs or symptoms. 1% of children had clinically important injuries, requiring neurosurgery or hospitalization for >1 night, and 5% had any traumatic brain injury. Notably, 68% of infants had risk scores <5 and none of these had clinically important injuries. 48% of infants had scores <4 and none of these children had any injury on CT. Interestingly, 23% of the CTs obtained on infants in the original PECARN study were on children with scalp scores <4 and therefore could have been avoided.
This study validates the high performance of the scalp risk score for infants with isolated scalp hematomas. When a child is classified as medium risk by PECARN based on the presence of a scalp hematoma, the scalp risk score can be calculated to determine their risk of injury more accurately. Nearly half of children will have risk scores <4 and not need to undergo CT. Younger infants with large hematomas in their temporal or parietal regions are higher risk and often require CT acquisition.
For your patient with an isolated scalp hematoma, you calculate their scalp score of 3 (age of 6 months= 1 point; size of 0.5cm= 1 point; occipital location= 1 point), placing them at very low risk of any brain injury. They can be discharged from the ED safely with return precautions.